Ontario Animal Health Network (OAHN) Public Health Update 2023
What is the OAHN Public Health Update?

The Ontario Animal Health Network (OAHN) was created to achieve coordinated preparedness, early detection, and response to animal disease in Ontario. OAHN is a “network of networks” with individual networks for different species/sectors, each of which involves collaboration among veterinarians, animal owners and stakeholders in the field with laboratory, academic and government experts. This annual update was created especially for public health professionals in Ontario, to highlight pertinent topics from the last 12 months from the OAHN companion animal and other species networks, and to help strengthen the link and communication between animal health and public health networks.
Network Highlights 2022-2023
HPAI in a dog, cats (S1 2023)
In late March, highly pathogenic avian Influenza A(H5N1) HPAI virus was isolated from samples taken from a dog in Durham Region that passed away several days after being found scavenging a dead goose that also tested positive for the virus. Since then, three feral cats with severe respiratory / neurological signs in Peel Region and Lambton County also tested positive for H5N1 virus. It is considered likely that the infection contributed to the death of these animals.
HPAI infection should be considered in dogs and cats that may have direct contact with wildlife, and/or scavenge sick or dead birds or other animals. Dogs are also susceptible to other strains of Influenza A(H3N2), and may be at risk from contact with other dogs in, or that have travelled to, high-risk areas abroad. PCR testing for Influenza A is available through veterinary diagnostic labs in Ontario. Any influenza strain in a companion animal is immediately notifiable and will be reported by Ontario laboratories to both OMAFRA and the Ontario Ministry of Health.
OAHN Project: H5N1 HPAI – feral cats (S2 2023)
As H5N1 influenza continues to be found in an increasing array of wild and captive mammals (including domestic cats in Poland and shelter cats in South Korea, potentially linked to feeding of contaminated raw poultry, as well as fur farms in Spain and Finland), scientists remain on alert for genetic mutations in the virus that may allow it to transmit more easily between mammals, and potentially spillover more easily into people.
Current science indicates that the risk of humans contracting highly pathogenic avian Influenza A(H5N1) HPAI virus continues to be very low. Nonetheless, owners are encouraged to take appropriate precautions to protect their pets and themselves by avoiding direct and indirect contact with sick or dead wildlife, especially migratory birds.
The latest detection of H5N1 in Ontario was in June 2023, but it is anticipated that viral activity will increase again in the fall as migratory birds fly south through this region once again.
The companion animal and wildlife OAHN teams are collaborating on a joint pilot project beginning this fall to help shed some light on the potential level of exposure and range of clinical disease due to H5N1 influenza in primarily outdoor / feral cats that are more likely to have contact with infected wild birds. Watch for updates on the OAHN website and social media over the fall and spring migration seasons!
More echinococcosis (Q4 2022, S1 2023)
In the last decade, it has become clear that Echinococcus multilocularis (EM) is now endemic in wildlife in southwestern Ontario. This was demonstrated yet again by the finding of a chipmunk with alveolar echinococcosis (AE) in Durham region last fall, and in another dog in the Hamilton region this spring. Fortunately infection in Ontario dogs remains rare (or at least rarely diagnosed) and even more rare in people, but particularly due to the insidious nature of AE, it is crucial that we keep this disease on everyone’s radar. At least 2 cases of AE were detected in people in Ontario in 2022. Remember: infected people develop AE, but they can only be infected by ingesting eggs from canid feces. Dogs are typically infected by ingesting tissues from infected small mammals and develop intestinal infections, but occasionally can also develop AE from ingesting large numbers of eggs! Check out the OAHN EM infographic or the 2022 OMAFRA veterinary update on EM risk in Ontario.
Update: Lyme disease infographic (S2 2023)
OAHN has updated its infographic for veterinarians on ticks and Lyme disease in Ontario with the latest risk area map for Ixodes scapularis from PHO. It has quick tips on monitoring, screening, and when not to treat dogs. Also check out the OAHN tick checklist for pet owners!
More on blastomycosis (Q3 2022, S1 2023)
In the spring of 2022, a veterinarian advised OAHN of a cluster of 4 ocular blastomycoses (blasto) cases in Eastern Ontario. Infection in the dogs was confirmed by urine antigen test or other signs of systemic fungal infection (e.g. on thoracic radiographs). There has also been recent concern about increased cases of blasto in people in southwestern Quebec. In the fall of 2021 there was a large outbreak of blasto in people in the First Nations community of Constance Lake ON. Increasing cases of blasto in both people and animals have been reported in Minnesota for the last several years. This has all led to renewed interest in surveillance of pets and/or wildlife to help detect high-risk areas for this typically regional or travel-associated disease.
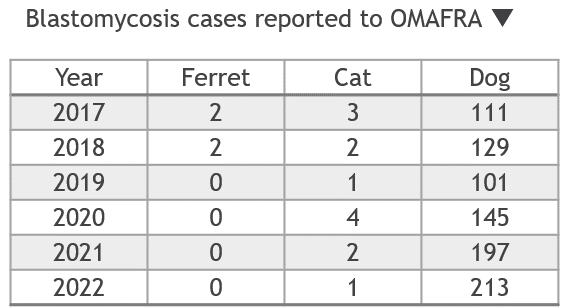
In an effort to learn more about the situation with blastomycosis across Ontario, the 2023 OAHN spring survey asked some specific questions about how and how often clinics are diagnosing this infection:
- Approximately 10% of respondents diagnosed cases in dogs in the last 12 months, compared to 2% in cats.
- 49% of respondents diagnose infection based on some combination of history, clinical signs, radiographs, in-house cytology and urine antigen testing – these cases would NOT be included in OMAFRA’s annual notifiable disease summary because they do not involve an Ontario laboratory.
- Other comments included suspicion of cases linked to a local excavation site, and cases in smaller breed dogs (compared to more typical cases in large breed dogs.
Salmonella and raw food diets (RAIZO 2023)
A report shared with OAHN by our counterparts in Quebec (RAIZO) also bears mentioning here. From 2020 to 2022, an outbreak of 17 human cases of multidrug-resistant Salmonella (I:4,5,12:i:−) was identified in Quebec. The majority of these cases involved children aged two years or younger. Of 14 cases investigated, 8 (57%) had direct contact with a dog fed a raw meat diet. For the six other cases investigated, direct or indirect contact with cattle or consumption of beef were reported. The situation also highlights the public health risks associated with raw meat diets for pets.
Aquatic: Piscine lactococcosis project (Q1 2023)
Piscine lactococcosis is a trio of bacteria – Lactococcus garvieae, L. petauri and L. formosensis. It’s been emerging issue in the Ontario salmonid population in the last several years and is expected to continue as a problem due to climate change warming waterbodies and creating longer periods of time for disease to spread and flourish. It causes a rapid septicemic disease with high mortality in fish when water temperatures are 15C or higher. The industry has developed an autogenous bacterin to try to manage mortality, but we still don’t know what is out there and how widespread these bacteria are. They are also emerging as a human pathogen associated with the consumption of contaminated aquatic animal products. The OAHN Aquatics network has therefore initiated a project to help determine the baseline prevalence of this pathogen trio in Ontario salmonid facilities. Watch the OAHN website for project updates in the next year!
Equine: Wildfire smoke (Q2 2023)
Wildfire smoke was a health hazard for horses in early summer 2023, with many equine veterinarians fielding questions from owners regarding appropriate intensity and duration of exercise based on the air quality. As with people, inhaling wildfire smoke leads to a range of outcomes in horses from mild respiratory irritation to lung inflammation, aggravation of asthma and reduced lung function. Smoke not only affects the quality of life for many horses but has particular implications for equine athletes. Excessive coughing was the most common clinical sign reported by veterinarians managing equine athletes in areas with poor air quality. Equestrian Canada recommends cancelling equine sporting events at an air quality health index (AQHI) of 10 to protect equine health, whereas the Sports Information Resource Centre (SIRC) recommends an AQHI of 7 for human athletes. Ontario racetracks used an AQHI of 8 to recommend cancellation of races and/or training. Notably Ottawa had days when the AQHI was much greater than 10.
Other: Chlamydia psittaci, pet birds (Q1 2023)
Outside of the OAHN networks, in 2023 the OMAFRA co-leads for the OAHN poultry and alternate species networks have been working with Ontario public health units and private veterinarians on an increasing number of Chlamydia psittaci cases in exotic pet birds. Spread of C. psittaci may be linked to movement of birds between collectors and a general increase in pet sales (including birds) through the pandemic. Birds most often carry C. psittaci subclinically, but in some cases can cause severe disease including hepatitis, diarrhoea, weight loss and death (avian chlamydiosis). While birds are the primary hosts, C. psittaci can infect a range of mammals, including humans (causing psittacosis, or “parrot fever”). It is immediately notifiable to both OMAFRA and local public health.
OAHN Project: Rabies titres, imported dogs (S2 2023)
The World Organization for Animal Health recommends a rabes antibody titre (RAT) of >0.5 IU/mL for dogs travelling internationally, to demonstrate that a dog has responded to rabies vaccination. However, vaccines must be administered according to label directions to help ensure protection from infection, regardless of a dog’s RAT. Dogs imported to Canada require a valid rabies vaccination certificate, but not a RAT test. Other studies have shown that RATs are highly variable even among dogs with current rabies vaccination certificates, and many dogs do not meet the recommended minimum RAT threshold.
- Median RAT for all dogs was 0.6 IU/mL
- 48% of dogs had titres below the recommended level of 0.5 IU/mL
- 28% of dogs had no detectable titre
Possible reasons for low titres:
- Not vaccinated / falsified certificate
- Ineffective vaccine product used
- Mishandled vaccine product used
- Poor individual response to vaccine (e.g. concurrent illness)
These results reinforce the reason behind the legal requirement for dogs, cats and ferrets from outside Canada or the US to be revaccinated for rabies upon arrival, to ensure they have adequate protection against this deadly virus. Click here for a 1-page summary of the study results.
Need-2-Know video: Rabies in Pets (Q4 2022)
Check out the latest whiteboard video from OAHN! Narrated by Pogo the rescue dog, this 4.5 minute video helps explain to pet owners some important basics of how rabies infection works and the importance of vaccination, as well as why vaccination or antibody titres can’t necessarily eliminate the risk of rabies in dogs from high-risk areas (either in Canada or outside Canada). Feel free to share the video on social media or other platforms!

Rabies reg update (S1 2023)
On July 1, 2023, two important regulatory changes came into effect regarding rabies:
- HPPA Reg 557: Public health units will have the authority to order rabies testing of any deceased dog, cat or ferret when a person was potentially exposed to the animal’s saliva within 10 days prior to death.
- HPPA Reg 567: A rabies vaccine approved for use in either Canada or the US and administered by a licensed veterinarian from either country (or their delegate) will be considered valid in Ontario.
Wildlife rabies update
Rabies response and control in Ontario is a joint effort involving the public, animal owners, veterinarians, animal and wildlife control organizations, public health units, the Ontario Ministry of Agriculture, Food and Rural Affairs (OMAFRA) and the Ministry of Natural Resources and Forestry (MNRF). Click here for MNRF’s new interactive Ontario rabies surveillance map. Annual maps of rabies cases in Ontario (including terrestrial rabies and bat rabies cases) are available at www.ontario.ca/page/rabies-cases.
Remember that ANY direct contact between a pet and a live bat is considered a potential rabies exposure, and ALL* dogs and cats – even if currently vaccinated – require a rabies booster within 7 days of an exposure unless the bat can be tested (and is negative) within this window.
NEVER put a live bat in the freezer. Contacts for humane euthanasia of bats (and other animals for rabies testing) can be found on the OAVT Rabies Response Program (RRP) website.
Additional detailed rabies response information for veterinarians is available on the recently updated webpage, www.ontario.ca/page/rabies-information-veterinarians.
| Confirmed wildlife rabies cases in Ontario, Dec 2015 – Aug 2022: | ||||||||||
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | Total | |
| Raccoon-variant | 10 | 255 | 119 | 65 | 22 | 9 | 14 | 23 | 6 | 523 |
| Fox-variant | 1 | 3 | 10 | 7 | 0 | 0 | 0 | 0 | 0 | 21 |
| Rabid bats | 0 | 29 | 20 | 31 | 41 | 39 | 27 | 35 | 13+ | – |
To date, all raccoon-variant rabies cases since 2022 have been detected in the St. Catharines area. Rabies was also detected in a pet cat in St. Catharines in 2023, but the strain could not be typed.
The MNRF distributes oral rabies vaccine (ORV) baits to help limit further spread of rabies in raccoons, skunks and foxes (there is currently no effective means of controlling rabies in bats). Over 8.3 million ORV baits have been distributed since December 2015, and the MNRF has performed close to 30 000 dRIT screening tests as part of their surveillance efforts. The 2023 rabies control operations are currently underway.
REMEMBER: Owners who have a concern about potential exposure of one of their animals to rabies should always be referred to their local veterinarian FIRST. Veterinarians seeking assistance with a rabies risk assessment or animal testing should contact OMAFRA using the online rabies response request form (http://www.omafra.gov.on.ca/rabiesrequest), or at 1-877-424-1300.
Updates to notifiable disease list, Ontario
Changes to the list of animal diseases that are immediately and periodically notifiable in Ontario under the Animal Health Act (2009) came into effect on 01-Feb-2023. The update included clarification of some of the pathogens and diseases already on the lists, some adjustments to which hazards are periodically notifiable (i.e. reported annually by diagnostic laboratories in Ontario) versus immediately notifiable (by either the veterinarian or laboratory involved), and the addition of some hazards including Echinococcus multilocularis, Campylobacter jejuni, Chlamydophila psittaci, SARS-CoV-2, Toxoplasma gondii and Leishmania spp. Deletions included giardiasis.
OAHN disease reporting portal
Ontario veterinarians can report unusual companion animal infectious disease cases to OAHN any time using the online disease reporting portal on the OAHN companion animal homepage. Submissions will be reviewed by members of the network team to detect any notable disease patterns and occurrences that should be communicated to Ontario veterinarians.
Please note that listed notifiable or reportable diseases must still be reported to the appropriate provincial or federal animal health or public health authorities.
In this issue
- What is the OAHN Public Health Update?
- HPAI in a dog, cats (S1 2023)
- OAHN Project: H5N1 HPAI – feral cats (S2 2023)
- More echinococcosis (Q4 2022, S1 2023)
- Update: Lyme disease infographic (S2 2023)
- More on blastomycosis (Q3 2022, S1 2023)
- Salmonella and raw food diets (RAIZO 2023)
- Aquatic: Piscine lactococcosis project (Q1 2023)
- Equine: Wildfire smoke (Q2 2023)
- Other: Chlamydia psittaci, pet birds (Q1 2023)
- OAHN Project: Rabies titres, imported dogs (S2 2023)
- Rabies reg update (S1 2023)
- Wildlife rabies update
- Updates to notifiable disease list, Ontario
- OAHN disease reporting portal
Companion Animal Network Team:
- Eastern ON: Dr. Julie Calvert
- Southern ON: Dr. Emma Webster
- Northern ON: Dr. Hailey Bertrand
- GTA ON: Dr. Donia Eino
- Animal Health Lab: Dr. Kris Ruotsalo, Dr. Emily Brouwer
- Ontario Vet College: Dr. Scott Weese, Dr. Shauna Blois, Dr. Allison Collier
- OMAFRA: Dr. Maureen Anderson, Dr. Hannah Golightly
- Network coordinator: Dr. Tanya Rossi


